A deep dive into rheumatoid arthritis
How researchers are using Standard BioTools technologies to gain insights into disease pathophysiology
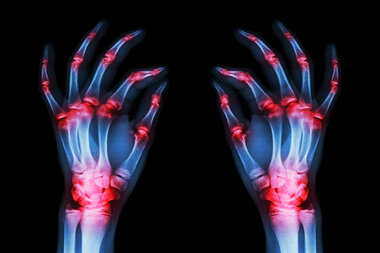
Rheumatoid arthritis (RA) is an autoimmune condition that causes pain and inflammation in the body’s joints. The immune system attacks the synovium (the lining of the joints), leading to inflammation, stiffness, swelling and pain that usually affect the hands, knees or ankles but can also cause issues with the eyes, heart, circulatory system and lungs.
Chronic inflammatory diseases are the most significant cause of death in the world, and the WHO ranks chronic diseases as the greatest threat to human health. RA is the most common chronic inflammatory joint disease and is a leading cause of disability globally. In 2019, 18 million people worldwide were living with the condition, suffering from mobility issues and physical weakness that impact their everyday lives and general well being. Untreated RA can lead to serious joint damage, complications in the major organs and a reduced life expectancy.
The cause of RA is unknown, and currently, there’s no cure. While no single laboratory test can accurately diagnose RA, understanding the dynamics of the immune system is key for early identification and effective disease management, which can reduce the severity of symptoms, slow the progression of RA and potentially prevent or lessen the chance of disability. Employing effective, efficient tools and technology can help researchers gain deeper insights into the disease’s pathophysiology and potentially improve standard of care and quality of life for those with RA.
Standard BioTools™ platforms enable deeper insights into the immunological landscape of RA and further research into the disease:
- Ibáñez-Costa et al. characterized splicing machinery (SM) alterations in leukocytes of patients with RA and assessed SM influence on their clinical profile and therapeutic response. Leukocyte subtypes from 129 patients with RA and 29 healthy donors were purified, and a 48.48 Dynamic Array™ integrated fluidic circuit (IFC) was used to assess the expression of 45 selected transcripts of the major and minor spliceosome and associated splicing factors. The team found altered expression of several SM elements in RA leukocytes, with eight elements equally altered in all leukocyte subtypes. This signature has the potential to classify high disease activity and identify patients showing atheroma plaques. IgG anti-citrullinated protein antibodies from patients with active RA modulated the expression of SM elements in healthy donor leucocytes in vitro, suggesting a key role for these antibodies in SM element alteration and inflammation. Furthermore, anti-TNF therapy in RA patients reversed expression of the SM elements in responders.
- A recent clinical study (BioRRA, NCT02219347) described in Nature Medicine leveraged CyTOF™ technology to investigate immune signatures associated with RA flare after withdrawal from disease-modifying anti-rheumatic drugs (DMARDs). DMARDs are potentially toxic, which means they require expensive, labor-intensive monitoring and can be seen as a limit to an otherwise normal lifestyle; DMARD minimization strategies could improve quality of life for those with RA while reducing drug toxicity as well as costs and healthcare resources. The researchers therefore wanted to identify reliable remission and flare biomarkers to help inform personalized approaches to DMARD therapy. Using a 41-marker CyTOF panel in addition to multiplexing, investigators identified three circulating cellular subsets in PBMC samples from 36 participants in the BioRRA study at baseline and follow-up – CD45RO+PD1hi CD4+ and CD8+ T cells and CD27+CD86+CD21– B cells – that signaled the onset of arthritis flare. These key insights provide further understanding of the immune mechanisms leading to flare and maintenance of remission in RA.
- Research by Hansen et al. aimed to provide comprehensive immunophenotyping of people with RA in an effort to help reveal the mechanisms underlying RA pathogenesis. The team analyzed deep immunophenotyping data from 52 people with RA and 47 healthy controls (HC). Whole blood samples were stained with the Maxpar™ Direct Immune Profiling Assay and stabilized with Prot1 stabilizer, according to a previously validated workflow, then acquired with a Helios™ mass cytometer. The CyTOF workflow provided a high-dimensional approach to detecting marker combinations and cluster generation and resulted in the team gaining a deeper immunophenotypic understanding of the RA landscape. The researchers observed a significant disparity in immune cell profiles between people with RA and HC, notably a reduced frequency of CD27+IgD+ unswitched memory B cells in RA. These results reveal that the reduced frequency of unswitched memory B cells in people with RA is the only significant abnormality distinguishing RA from HC in a complex immunophenotyping panel of 72 different cell populations.
As the epidemic of chronic inflammation and autoimmune diseases continues to grow, the importance of timely and accurate diagnosis does, too. Using versatile next-generation tools to glean a better understanding of immune response to RA can help shed light on the development of this poorly understood disease and potentially open avenues for further research focused on treatment and prevention.
Unless explicitly and expressly stated otherwise, all products are provided for Research Use Only, not for use in diagnostic procedures. Find more information here.
